Just 9 per cent of men born today can expect to reach retirement age in good health, warn IPPR and Future Health
14 Jun 2022Press Story
- Only 16 per cent of women born today can expect to reach state retirement age in reasonable health
- Experts call for overhaul in approach to healthcare in England
A new report from IPPR and Future Health calls for major reforms to put the NHS on a more sustainable footing after the shock of the pandemic.
This call for reform also comes as new analysis shows that just 9 per cent of men and 16 per cent of women born today can currently expect to reach state retirement age (rising to 67 by 2028) in good health. The findings show that the vast majority of people have a ‘healthy life expectancy’ lower than the state pension age.
The research also shows a clear place-based inequality, with those people living in the wealthiest local authorities more likely to have a healthy life expectancy that exceeds the pension age. People born in areas with the highest rates of multiple deprivation, like Blackpool and Nottingham, can expect to fall into poor health well over a decade before the state retirement. Moreover, given lower household incomes in these areas, they may have less means to cope if and when a shock diagnosis strikes.
The researchers argue that this is a symptom of the country’s stark health inequalities, that stand to deepen in the wake of the Covid-19 pandemic, unless urgent action is taken to revitalise the NHS. The report warns that a failure to do so would mean declining health outcomes, a weaker economy, and increasing public disillusionment in politics.
IPPR and Future Health call on all political parties to make NHS sustainability a priority, to ensure more people can live more of their lives in good health. Achieving this means ensuring that NHS can continue to improve population health, in line with what the latest public health, science and innovation make possible.
While the right level of funding is identified as a precondition for sustainable healthcare, the report argues that more money devoid of a reform agenda would be unlikely to deliver improved health outcomes.
Drawing on the lessons of the pandemic and evidence submitted by senior doctors and health leaders, the report sets out practical steps for NHS reform:
- Investment – Health should be seen as an enabler of greater prosperity and a strategic investment by the Treasury. Health indicators should become as important as GDP when assessing policy, and all departments should undertake have health impact assessments when designing policy. Investment in prevention and new life sciences innovation should be focused on tackling health disparities between places.
- Tackling health inequality – The NHS funding formula should be adjusted to better direct funds to areas with greater levels of economic deprivation. The NHS should also start setting ambitious health inequality targets for different illnesses, and should expand the use of community diagnostic hubs and primary care facilities.
- Ending the innovation postcode lottery – The latest medical treatments and technologies are not currently being rolled out evenly across the country. The NHS should set out a new mission-based approach to innovation, based on improving health outcomes and tacking health disparities overseen by the NHS Transformation Directorate. A new national health infrastructure fund should roll-out new data infrastructure that can enable the adoption and scale of new innovation and technology.
- Integrated, personalised care – Ensuring all aspects of the health system work together better is key to improving patient outcomes and experience. Building on the existing Integrated Care Systems that have started this work, the NHS should also develop plans for a more integrated and diverse workforce that means health professionals can provide more personalised and coordinated care to patents as they move between different health and care services.
Chris Thomas, IPPR principal research fellow, said:
“It’s shocking that so many people don’t even make it to retirement age before the effects of ill health start to take a toll on their lives. The fact that it is the poorest that are likely to suffer ill health earlier shows that this is preventable. Ensuring more people can live more of their lives in good health is possible, and a key part of this is ensuring we have a sustainable NHS, capable of improving population health even in hard times.
“Brilliant care is still possible within our NHS. The solution to the sustainability challenges it faces is unlikely to be a wholescale shift in operating model, as some suggest. Marketisation or insurance-based models are not silver bullets and pursuing them at the expense of more important reform priorities could well make things worse. Instead, the search should be for policies that can help the NHS both universalise and sustain the best care for all. It’s time to revitalise our NHS.”
Richard Sloggett, research director and founder of Future Health and former advisor to the secretary of state for health and social care, said:
“The pandemic has shown us that health is our most important personal and national asset and that good health is too unevenly distributed across the country. As part of the pandemic recovery, political and health leaders now need to set a new direction for delivering a higher quality and more equitable health system. Setting health as a strategic national investment priority that can support wider improvements in societal, community and economic regeneration will be an important step-change in approach.
“This report shows that good ideas in health are not based on a particular political ideology, but rather on identifying what works best and then using the reach of our healthcare system to scale the solutions to improve health outcomes and tackle health inequalities. If the government want to achieve their aspiration to build back better, and deliver on the promises linked to the new health and social care levy, then these ideas provide an immediate blueprint.”
ENDS
Chris Thomas and Richard Sloggett are available for interview
CONTACT
David Wastell, Director of News and Communications: 07921 403651 d.wastell@ippr.org
NOTES TO EDITORS
- The IPPR paper, Sustainable healthcare: Practical steps to build back better in the English NHS by Chris Thomas and Richard Sloggett, is published from 0600 on Tuesday June 14. It will be available for download at: http://www.ippr.org/research/publications/sustainable-healthcare
- Local authority healthy life expectancy data available on request
- Figure 2.1: There are large disparities in healthy life expectancy and the proportion of life lived in good health in England today.
Chart shows data (as dots) plotted by local authority.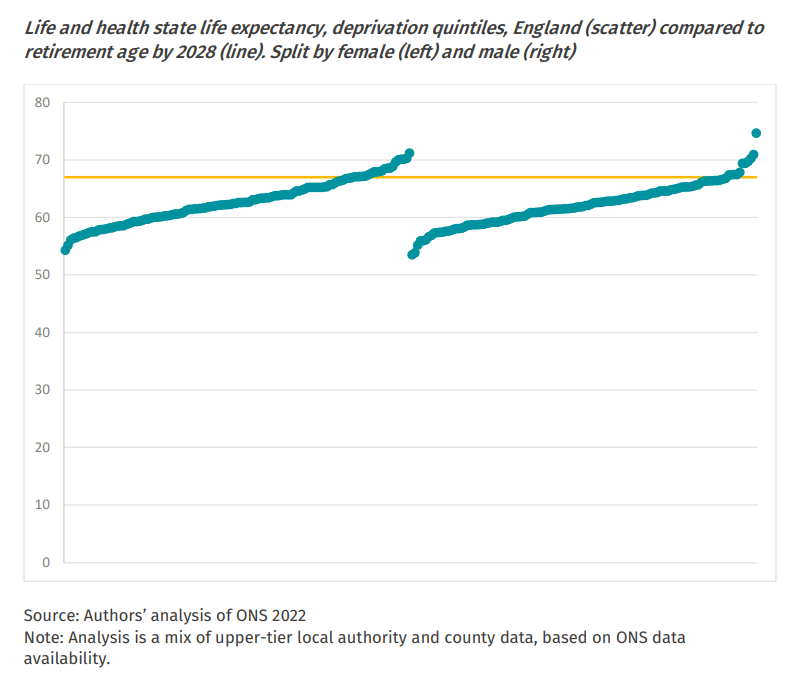
- The figures for those who can expect to live to state retirement age are derived from comparing healthy life expectancy at birth with the state retirement age. The state retirement age is set at 67 for men and women, which it is scheduled to reach in 2028. Analysis uses healthy life expectancy at birth.
- ‘9 per cent of men born today can expect to get to state retirement age in good health’ calculated as follows:
a) Healthy life expectancy at birth assessed by local authority (upper-tier and county data)
b) Healthy life expectancy >67 coded 1, healthy life expectancy <67 coded 0
c)Share of <1-year-old male population of local authorities with a healthy life expectancy over 67, compared to <1-year-old male population of England as a whole
d) ‘Expect’ refers to the fact that figures are local authority averages – and that, in any given place, individuals may realise much higher or much lower healthy life expectancies.
The equivalent method has been used to establish the finding that 16 per cent of women born today can expect to reach state retirement age in good health. - Our analysis uses known trajectories on increases in the state retirement age. This means we assume that policy decisions do not lead to rises above the age of 67 after 2028. This may make our estimate conservative – rises in the state retirement age may be more likely than decreases in coming decades.
- IPPR is the UK’s pre-eminent progressive think tank. With more than 40 staff in offices in London, Manchester, Newcastle and Edinburgh, IPPR is Britain’s only national think tank with a truly national presence. www.ippr.org